Insurers cut back GLP-1 coverage as demand soars: Found study

By A Mystery Man Writer
As demand surges for GLP-1 therapies, insurers are pulling back on coverage, according to new data from obesity care provider Found. | Sarah Jones Simmer, CEO of Found, said that the trends are likely the result of irresponsible prescribing for recreational reasons causing the pendulum to swing "all the way in the other direction," and it's leading to patients who have genuine medical need struggling to access these therapies.

Weight loss drugs like Ozempic could upend industries including air travel - The Washington Post

3 Reasons ResMed's CEO Isn't Worried About Ozempic or Wegovy

Designing fiscally viable coverage of GLP-1 weight-loss drugs

PBMs, insurers restrict Ozempic, Wegovy, weight loss drug access

Ozempic: How the Diabetes Drug Works and Why It's Such a Big Deal for Weight Loss - WSJ

The Rise of GLP-1 Receptor Agonists and Coverage Challenges
Lilly weight-loss drug Zepbound new US prescriptions surpass

The Rise of GLP-1 Receptor Agonists and Coverage Challenges

Obesity Cooking with Kathy Man
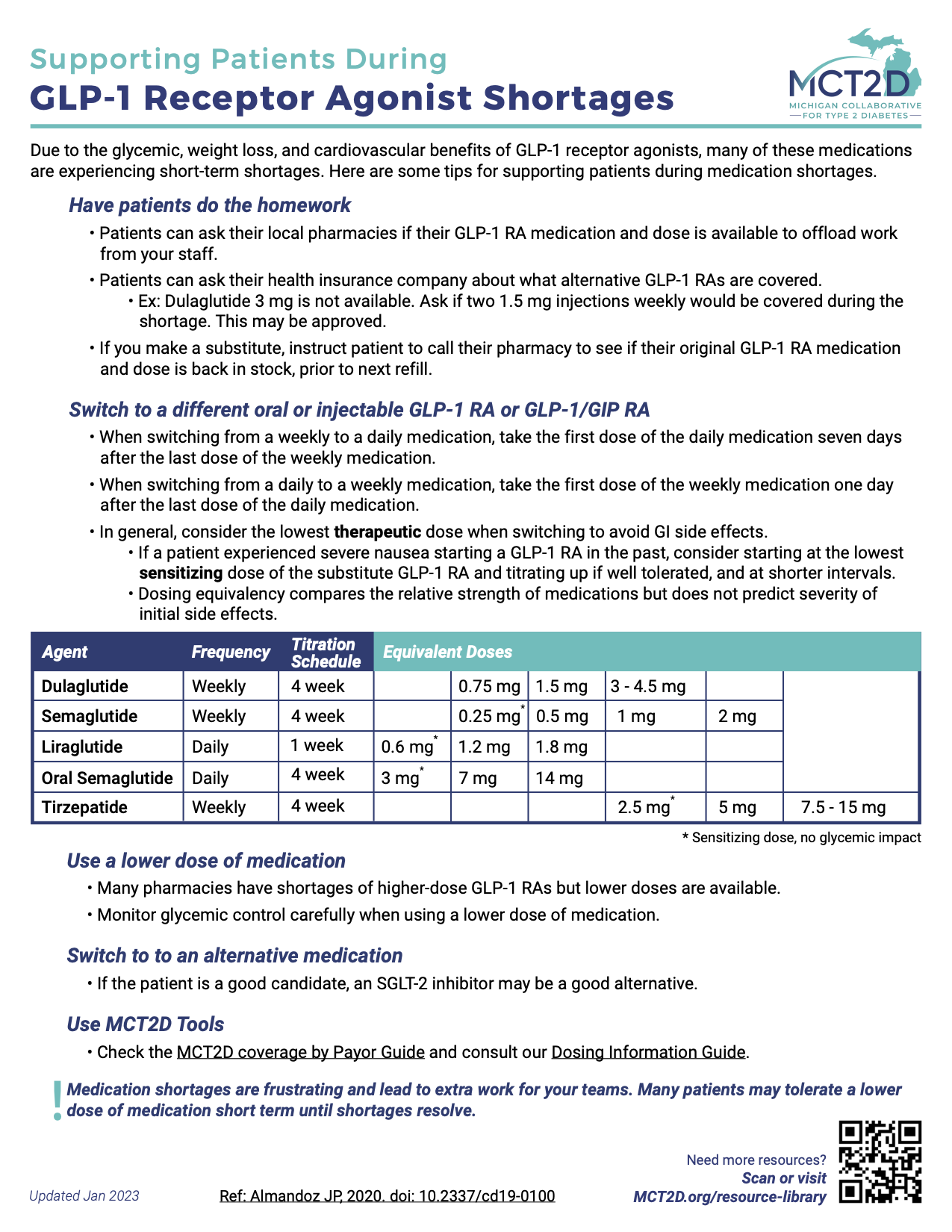
MCT2D 2023 Updates to Coverage for GLP-1 RAs, SGLT2 i's, and

Focus: US diabetes patients face delays as insurers tighten Ozempic coverage
- women yoga pants with pockets stretch workout running yoga leggings Prices and Specs in Singapore, 12/2023

- Tailored Mini Skirt in White

- Go Green on Earth Day and Every Day with B.R.A. Recycling - Lingerie Briefs ~ by Ellen Lewis

- VAMPIRE® MERLOT

- 3 pr lee jeans lot - clothing & accessories - by owner - apparel

:max_bytes(150000):strip_icc()/shortcovering.asp_final-950d1cb29a2b4fd9a1067a3af8ca886d.png)